Engaging patients in health care decision making can mean anything from collaborating on treatment plans, to designing waiting areas, to service users creating core policies for hospitals and medical schools. In the past five years, the Department of Psychiatry at the University of Toronto has begun the early stages of collaborating with service users in the production of curriculum, the training of staff and residents, policy development, and admissions. Much of this work has happened under the umbrella of “Pillar Four,” part of a series of goals set out by the department as part of their Strategic Plan in 2012. Pillar Four objectives include: addressing stigma, developing advocacy work for social responsibility, and increasing community and consumer input in departmental education.
InSight, a committee comprised of critical community stakeholder organizations and a representative of the department, was formed to provide advice and feedback to Pillar Four activities. Co-chairs Lucy Costa of the Empowerment Council at CAMH and Dr. Priya Raju, along with other members of InSight, have collaborated with the Department of Psychiatry combining critical reflection with an extensive history of consultation on psychiatric education and practices. In this report, we reflect on our own process in the development and work of InSight and in the creation of a collaboratively designed curriculum in the course, “Centering Madness.”
In discussions with five psychiatrists and one psychologist who are currently working with service users on various initiatives in the department, we explore the strengths and challenges of Pillar Four’s “Dialogue” mandate and draw from recent experiences of patient engagement. We focused on speaking with staff members about their experiences and impressions with an eye to identifying gaps in knowledge and areas in which resources could be better directed to support service user inclusion in departmental mandates.
In one of these conversations, a staff member commented on the ways patients engage in health care institutions outside of psychiatry, referring specifically to cancer patients who have physically transformed clinical spaces through choosing paint colours. While we respect and endorse any level of participation and decision-making that service users choose to undertake, we want to highlight the potential for service users to positively colour institutional practices beyond aesthetics. At the same time, we discuss how this potential can be limited by challenging dynamics that emerge when staff and service users work collaboratively as equals. In particular, when service users take leadership in collaborative initiatives, this dynamic can intensify. As such, in the final sections, we offer insights regarding staff learning needs with recommendations for future directions.
Excerpts from the report:
Five Questions to Assess Quality of Patient Engagement
- Were service users included at planning stage?
- Who does preliminary research to set up ground rules and context?
- Who manages the budget and decides how funds are allotted?
- When service users are engaged do they shape day-to-day decisions and outcomes?
- Are measures in place to assess and ensure accountability?
These five questions provide a basic starting point to address the ethics and efficacy of collaborations between professionals and service users. More than that, they offer an opportunity to create the kind of dialogue about power and process that is necessary to build strong relationships.
After Pillar Four: Recommendations for Ongoing Work
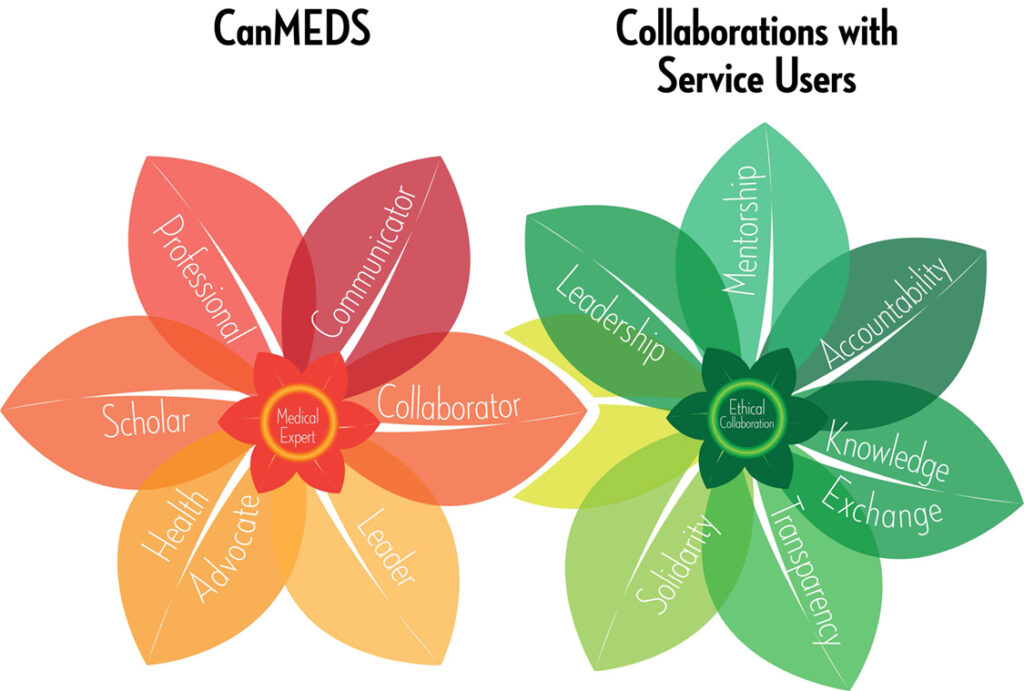
Left: CanMEDS diagram developed by the Royal College of Physicians and Surgeons of Canada to illustrate seven core competencies for doctors.
Right: InSight has created our own diagram, stemming from the “collaborator” role identified by CanMEDS, to illustrate the skills and framework required to ethically collaborate with service users
We offer our diagram as a framework for collaborations where service users can take the lead to create meaningful change. For service users, having their presence valued and their insight understood as leadership is a first step to redressing harm caused by histories of psychiatric care and past experience of collaborations with staff.
Citation information: Devaney, J., Costa, L., and Raju, P. More Than Paint Colours: Dialogue about Power and Process in Patient Engagement. (Toronto: The Empowerment Council, 2017).